By Brendan Pierson
(Reuters) – Health insurance plans run by U.S. states must cover gender-affirming surgeries for transgender people, a U.S. appeals court ruled on Monday.
The 8-6 opinion from the Richmond, Virginia-based 4th U.S. Circuit Court of Appeals upheld two lower court rulings, which had found that North Carolina’s state employee health insurance plan discriminated against transgender people by not covering surgeries for “sex changes or modifications,” and that West Virginia’s Medicaid program discriminated by excluding “transsexual surgeries.”
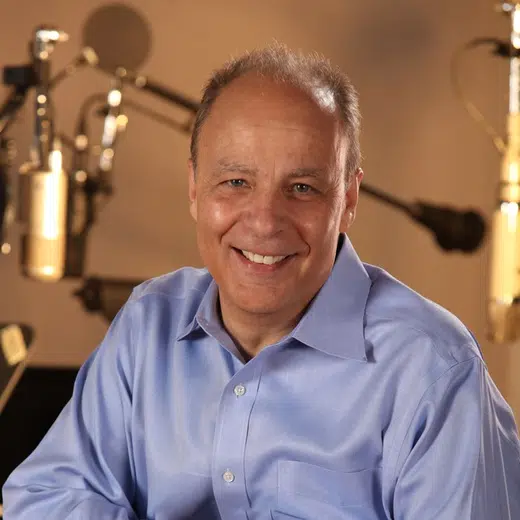
Circuit Judge Roger Gregory, who was appointed by Democratic former President Bill Clinton, wrote for the majority that such policies were “obviously discriminatory” because they did not cover medically necessary treatments for transgender people that they did cover for others. For example, he wrote, they would cover a mastectomy to treat cancer but not gender dysphoria, the distress caused by identifying as a gender different from the one assigned at birth.
North Carolina Treasurer Dale Folwell said in a statement that the state employee plan was “facing the real risk of looming insolvency” and “cannot be everything for everyone.” He said he would “follow every legal avenue available to protect the Plan and its members.”
West Virginia Attorney General Patrick Morrisey said the state would appeal to the U.S. Supreme Court.
“Our state should have the ability to determine how to spend our resources to care for the vital medical needs of our citizens,” he said.
The case began with separate lawsuits brought by transgender people challenging each state’s insurance program. The appeals were combined because they involved similar legal issues.
“The court’s decision sends a clear message that gender-affirming care is critical medical care for transgender people and that denying it is harmful and unlawful,” said Omar Gonzalez-Pagan, a lawyer at the LGBT group Lambda Legal, which represented the plaintiffs.
The states had argued that their programs’ exclusions did not discriminate because they were based on patients’ diagnosis and treatment, not transgender identity.
Gregory rejected that claim, saying the states’ basis for denying coverage was a “proxy” for discriminating against transgender people.
Circuit Judge Jay Richardson, who was appointed by Republican former President Donald Trump, wrote in a dissent that states “can reasonably decide that certain gender dysphoria services are not cost-justified, in part because they question the services’ medical efficacy and necessity.”
Monday’s ruling comes as part of a broader battle over healthcare for transgender people in the United States.
At least 22 Republican-controlled states have passed laws restricting gender-affirming care for people under 18, leading to legal challenges that have so far had mixed outcomes.
The U.S. Supreme Court earlier this month allowed Idaho to enforce its ban for now, while an Ohio court temporarily blocked a ban there.
(Reporting By Brendan Pierson in New York, Editing by Alexia Garamfalvi and Bill Berkrot)




Comments